Nurses to the rescue?
March 2, 2011 — As recently reported by Remapping Debate, little is being done to deal with the crisis in medical care that will result from the massive physician shortage that is just around the corner. Even if policy-makers begin to address this long-avoided challenge in the near future, the country will still feel the consequences of the shortage over the next decade, since it takes at least several years to ramp up an adequate and sustainable pipeline of new physicians.
So what can be done in the short-term? A leading proposal is to rely more on nurses as the physician shortage grows worse.
Advanced practice nurses — a category that includes nurse practitioners, nurse anesthetists, nurse midwives and clinical nurse specialists, and is often extended to include physician assistants — would be allowed to operate with greater autonomy, and, in some cases, entirely independently of physicians.
Currently, most states restrict what state licensing boards call “scope-of-practice” — that is, each state’s definition of exactly what types of care a specific license allows a nurse to perform.
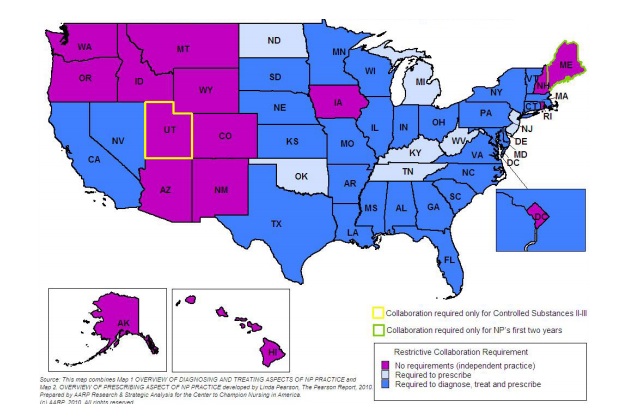
For example, many states — including California, Texas and New York — do not allow nurse practitioners to diagnose illnesses or prescribe medications without the direct supervision of a physician. In other states — like Michigan and Oklahoma — nurse practitioners are allowed diagnose, but not to prescribe. On the other hand, in 14 states — including Oregon, Montana and New Hampshire — nurse practitioners are allowed to do both without physician supervision. (See map at the bottom of the page.) Additionally, restrictions sometimes vary regionally within a state, with nurse practitioners practicing independently in rural areas and under the supervision of a physician in cities.
But the training for advanced practice nurses, who must earn either a master’s degree or a doctorate in their field, does not vary substantially from state to state, leading many to conclude that the varying scope-of-practice restrictions are caused more by political differences than by safety concerns.
Practicing at the top of one’s license
Advocates for removing scope-of-practice barriers in restrictive states argue that the limitations are illogical and wasteful, and that all nurses should be able to practice “at the top of their license” — meaning to the full extent of their training.
“I think the evidence is in place that given that we’re educating everybody to a particular level and they are passing certified exams, there is some waste of healthcare delivery capacity when states restrict the ability of nurses to practice at the top of their license,” said Catherine Gilliss, president of the American Academy of Nursing (AAN), a group that has long advocated for allowing nurses more autonomy.
This perspective was given a major boost last year, when the Institute of Medicine published a much-anticipated report called, “The Future of Nursing: Leading Change, Advancing Health,” which recommended, among other things, relaxing some state restrictions on nurses’ scope-of-practice.
Susan Hassmiller, the senior adviser for nursing at the Robert Wood Johnson Foundation and the study director for the report, said that there is no evidence indicating that quality of care suffers when advanced practice nurses work without physician supervision, and pointed out that the Institute of Medicine follows strict research standards when making recommendations.
Indeed, she said, research indicates that patient outcomes do not change dramatically regardless of whether a physician or an advanced practice nurse delivers primary care.
A patchwork of restrictions: state-by-state limitations on nurse practioners