June 8, 2011 — Remapping Debate has previously reported on attempts to “repeal” climate science; it appears that the U.S. agricultural industry’s widespread use of antibiotics in animals used for food is another area where science denial is at play. Even though the U.S. Food and Drug Administration, the U.S. Department of Agriculture, the Centers for Disease Control and Prevention, and the World Health Organization are united in concluding that such use leads to human exposure to antibiotic-resistant bacteria, the industry is actively fighting efforts to restrict the routine, non-medical use of antibiotics in animals, and the FDA has yet to impose a ban.
The problem — which the FDA and sister organizations say is a risk to public health — is already enormous, and it is growing. According to the CDC, Methicillin-resistant Staphylococcus aureus, an antibiotic-resistant bacteria commonly known as MRSA, kills an estimated 19,000 people per year in the United States. The cost of fighting antibiotic-resistant microbes exceeds $20 billion per year.
Medical misuse of antibiotics in humans is part of the problem. But another contributor is the misuse of the drugs in food animals. According to the FDA, a staggering 80 percent of the antibiotics used in the United States is used on livestock animals.
Livestock producers do not simply use antibiotics to treat sick animals. They also use antibiotics to promote growth or feed efficiency. The Union of Concerned Scientists estimates that 70 percent of the antibiotics used in the U.S. is used in food animals for non-therapeutic reasons — that is, for reasons other than treating disease. According to the FDA, 90 percent of the antibiotics given to animals is distributed via animal feed or water, a method that critics say is used primarily for non-therapeutic reasons.
A known problem
As early as the 1970s, the FDA recognized that the use of antibiotics in animals for non-therapeutic reasons could promote the development of antibiotic-resistant pathogens that are harmful to humans. In 1977, the agency proposed to withdraw approval for the use of two kinds of antibiotics — penicillin and tetracyclines —in animal feed at sub-therapeutic levels, or at doses too low to treat disease, because it said evidence showed the practice to be unsafe. But Congress recommended that further study be done on the issue and the FDA never acted on that recommendation.
Since then, the evidence showing that the use of antibiotics in animals for non-therapeutic reasons poses a health risk to humans has only gotten stronger. All the while, new strains of microbes that are resistant to an increasing number of drugs are continually discovered.
Scientists believe that antibiotic-resistant bacteria that originate in farm animals can transfer to human populations, either through animal handlers that then spread the pathogens to the general public, or via contaminated meat that is handled or eaten at home.
Scientific opinion is “overwhelmingly in favor of the fact that this broad use of antibiotics in animals is contributing to antibiotic resistant disease in humans,” said Margaret Mellon, director of the food and environment program at the Union of Concerned Scientists. “It just has to be the case. We use the same antibiotics in pork and in cows and in chickens as we do in doctors’ offices, and we’re generating these huge volumes of antibiotic-resistant bugs.”
Mellon summarized the prevailing scientific view that the non-therapeutic use of antibiotics in animals leads to human infections of antibiotic-resistant microbes in prepared testimony for a 2009 congressional hearing. The journal Clinical Infectious Diseases in 2002 wrote in a special supplement that the ‘‘[u]se of antimicrobials in food animals contributes to the growing problem of antimicrobial resistance in animal and human infections,” Mellon said. The World Health Organization in 2003 said ‘‘There is clear evidence of the human health consequences [from agricultural use of antibiotics, including] infections that would not have otherwise occurred, increased frequency of treatment failures (in some cases death) and increased severity of infections,” she added.
“The literature in this arena is voluminous and the conclusion is clear,” Mellon said in her prepared remarks. “Antibiotic overuse in agriculture — just as in human medicine — is undercutting the efficacy of important human therapies and generating more virulent pathogens.”
The USDA and the CDC have also come to acknowledge that the use of antibiotics in animals poses a health hazard to the public. Legislation to curtail the use in animals of antibiotics that are important for human medicine is supported by the American Medical Association, the American Public Health Association, the National Association of County and City Health Officials, and other organizations.
At the same 2009 congressional hearing, FDA principal deputy commissioner Joshua Sharfstein testified that the agency “supports ending the use of antibiotics [in animals] for growth promotion and feed efficiency,” and that doing so “will not compromise the safety of food.” In 2010, the agency released draft guidance recommending that the use of antibiotics in food animals be limited to uses “considered necessary for assuring animal health” and only when supervised by a veterinarian.
FDA inaction
Despite the evidence, the FDA has still not acted to force livestock producers to end the non-therapeutic use in animals of medically important antibiotics — that is, those that are used in human medicine.
Remapping Debate asked a spokeswoman for the FDA why the agency has not followed its own recommendations and imposed restrictions on antibiotics in food animals, and whether the burden placed on the national healthcare system and the threat to human health warranted immediate action to stem the risk of antibiotic-resistant microbes. In an emailed response, the spokeswoman did not answer the questions but said simply that the FDA is “currently reviewing the comments received [on the draft guidance] and determining the next steps.”
Lawmakers have also shown no willingness to address the problem. One bill that would eliminate the use of several classes of medically important antibiotics for non-therapeutic uses — the Preservation of Antibiotics for Medical Treatment Act of 2011 (PAMTA), introduced by Rep. Louise M. Slaughter, a Democrat from New York — has gone nowhere. (Slaughter introduced the same bill in 2009 as well, but it never even came to a vote in committee.)
Mellon said PAMTA is a well crafted bill, but it faces an uphill battle in Congress because of industry opposition.
“There is enormous opposition to it coming from the animal industry, which doesn’t want to start doing something about the problem,” Mellon said. “Basically they’re still in denial mode, that this is not a problem and therefore that they’re going to stop any legislation that would lead to a change in agricultural practices and they’re very powerful politically. They’re making it very difficult for the legislation to move forward.”
Danes take a different road
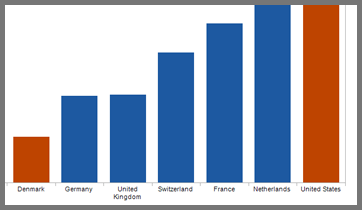
Denmark, the world’s largest exporter of pork, banned the use of antibiotics for growth promotion in animals in 1995 and banned all non-therapeutic uses of antibiotics in 2000. Denmark uses far less antibiotics per kilogram of meat produced than does the industry in the U.S. (see chart). Its experience shows that transitioning away from the non-therapeutic use of antibiotics in animals achieves a reduction in the level of antibiotic resistant bacteria found in animals, and that the shift can be accomplished without harming industry.
Per Henriksen, of the Danish Veterinary and Food Administration, testified at a 2010 congressional hearing that — 15 years after the ban on antibiotics used to promote growth — antibiotic use in livestock was still down 40 percent from pre-ban levels. Denmark uses more antibiotics to treat disease in animals than it did before the ban, since the animals are not fed a continuous dosage of drugs to ward off illnesses before they occur. But the decline in non-therapeutic dosages more than makes up for the difference.
The decrease in the usage of antibiotics has led to a measurable decrease in antibiotic-resistance in bacteria found in animals, Henriksen said. For example, resistance to macrolide antibiotics in campylobacter bacteria in pigs was reduced to 20 percent in 2006, compared with 80 percent pre-ban levels, he said. Resistance to vancomycin antibiotics in enterococci bacteria in broiler chickens was reduced to 5 percent in 2006 compared with a 75 percent resistance prior to the ban.
Antibiotic resistance in bacteria found in meat for consumption has also decreased, Henriksen said. In E. coli bacteria found in broiler meat, the incidence of resistance to cephalosporin antibiotics was less than 5 percent, compared with 35 percent in other EU countries, he said. At the same time, animal production in Denmark has increased, and animal health has not been compromised, Henriksen said.
Frank Aarestrup, director of the Antimicrobial Resistance and Molecular Epidemiology Unit at the Danish Food Institute said in testimony prepared for the 2009 hearing that there had been a gradual increase in the mortality of young pigs after the ban, but that rates had since fallen to pre-ban levels. In addition, the average number of pigs produced per sow, which he said was a key indicator of pig health and welfare, increased from 21 to 25 from 1992 to 2007, while overall swine production increased from 18.4 million pigs to 26.3 million pigs, a 43 percent increase, in the same time period.
Industry: there’s no proof!
The livestock industry denies that there is a link between the non-therapeutic use of antibiotics in animals and increased resistance to antibiotics in microbes infecting humans. Such a claim is “not based on any science,” said Dave Warner, spokesman for the National Pork Producers Council, a swine industry trade association.
Remapping Debate asked Warner if there was evidence that antibiotic use in animals leads to antibiotic resistant bacteria in animal infections. Warner conceded that there was. But he said there was no evidence that antibiotic-resistant bacteria in animals poses a human health risk.
Tara Smith, an assistant professor in the epidemiology department at the University of Iowa, said Warner’s argument ignored the fact that scientists are able to draw reasonable conclusions regarding human health risk based on the bacteria populations found in animals and humans.
A 2004 Government Accountability Office report summarizing the scientific evidence on the transfer of antibiotic resistance from animals to humans explained that “some studies have provided evidence of associations between changes in antibiotic use in animals and resistance to antibiotics in humans,” and that “studies that have examined the genetic makeup of the bacteria have provided evidence of a stronger link and have established that antibiotic-resistant campylobacter and salmonella bacteria are transferred from animals to humans.”
The report went on to note that a “small number of studies contend that health risks of the transference are minimal,” but pointed out that there are “many studies that have examined the genetic makeup of the bacteria [that] have provided evidence of a stronger link and have established that antibiotic-resistant campylobacter and salmonella bacteria are transferred from animals to humans.”
Warner said the scientific evidence did not demonstrate how the pork industry’s antibiotic use contributed to antibiotic resistance in humans. “We have never said that we are no part of the problem of antibiotic resistance,” he said. “We don’t know what, if any, part we are.”
Given the substantial risks antibiotic-resistant bacteria pose to public health, however, would it not be better to err on the side of caution in case the industry is making the problem worse?
Warner would not contemplate that circumstance, instead repeatedly reciting a different “what if” (that is, if, contrary to all scientific expectations to date, a consensus were to emerge that there is absolutely no link between industry practice and human health hazard, after the industry had been restricted). Banning the non-therapeutic use of antibiotics in animals would be costly to producers, he said.
Warner cited a 1999 Iowa State University study that concluded that the initial cost to producers of a ban on animal feed-grade antibiotics would be $6 per pig, and the industry would lose about $1 billion per year in profits. Increased costs would come partly from the need for additional troughs and space for pigs, the report said.
Sub-therapeutic doses of antibiotics allow livestock to be kept in more cramped in confined conditions because antibiotics make them resistant to the diseases they would otherwise contract in such close quarters. Additional veterinary treatments and longer weaning times for pigs would also add to costs, the study said.
But what if there were no cost to livestock producers to transitioning away from the non-therapeutic use of antibiotics? The federal government spends about $5 billion per year in so-called direct payments to farmers for growing crops, regardless of the crops’ market prices (other payments go to farmers if the price drops below a certain level or if natural disasters cause crop loss).
The direct payments are seen as wasteful and rife for elimination by both parties. Rep. Paul Ryan’s budget plan, for example, proposes cutting subsidies to farmers by $30 billion over 10 years, mostly through a reduction in direct payments. What if a fraction of that went to assisting livestock producers with curtailing the use of antibiotics?
Remapping Debate posed the question to Liz Wagstrom, chief veterinarian for the National Pork Producers Council. She said she thought producers would still resist, as they would be reluctant to give up what she said was a “tool to help produce healthier animals.”
Continue down the same path?
Warner said there is no evidence to show that the Danish ban on non-therapeutic uses of antibiotics has led to a public health benefit. Some studies have concluded that antibiotic resistance in human bacteria infections has not improved.
Mellon of the Union of Concerned Scientists responded that an immediate, sharp decline in antibiotic resistance disease in humans was not to be expected. “One of the problems with antibiotic resistance is that once you’ve generated it, if you withdraw the use of the antibiotics the traits don’t necessarily go away, they hang around in the bacteria,” she said. “You can’t expect that having generated this big problem that if we quit using antibiotics that we’ll return to a day when all of our pathogens were susceptible to drugs. That just won’t happen.”
But that is not an argument for not curtailing antibiotic use, Mellon said. “Of course the first rule of holes is when you’re in one you quit digging,” she continued. “From a public health standpoint what you want to do is not make the problem any worse.”